While the demand for healthcare services continues to rise with the aging of the Baby Boomer generation, the increased demand also comes with greater complexity. There are many challenges and obstacles preventing modern medical practices from maximizing their revenue potential.
One of the biggest sources of these obstacles is the healthcare revenue cycle. There are four main ways practices commonly struggle with revenue management:
- Low collection rates
Research shows that by 2019, nearly one-third of patient revenue may go uncollected and written off as a tax deduction. There are several reasons for this – some will be addressed below – but broadly speaking, one of the most significant is the rise of patient responsibility. Deductibles and copays have steadily increased over the last several years and show no signs of slowing down. Practices that already struggle with patient revenue collection must take action before the problem gets worse.
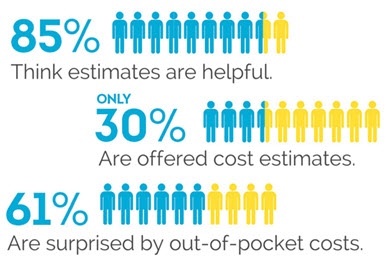
- Patient confusion
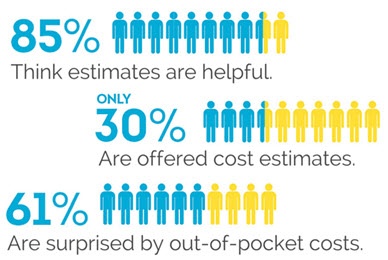 Between medical jargon, reimbursements from insurance companies, and changing healthcare legislation, it’s difficult for patients to fully understand their healthcare bills. Over 60% of all patients say that their bills confuse them – and since they are often sent an adjusted bill after the initial version, nearly 4 out of 10 patients don’t pay their medical bill right away, prioritizing other bills like housing and utilities. If patients receive a clear, accurate bill that they know will not change, they are more likely to pay.
Between medical jargon, reimbursements from insurance companies, and changing healthcare legislation, it’s difficult for patients to fully understand their healthcare bills. Over 60% of all patients say that their bills confuse them – and since they are often sent an adjusted bill after the initial version, nearly 4 out of 10 patients don’t pay their medical bill right away, prioritizing other bills like housing and utilities. If patients receive a clear, accurate bill that they know will not change, they are more likely to pay.
- Payment assurance
It’s always better for medical practices to collect payment from patients upfront – it’s notoriously difficult to secure payment once the patient leaves the office. But too many medical practices have no way to confirm that they will collect from patients, even if they are owed money upfront in the form of copays or patient deductibles. To solve this, healthcare offices need a system of payment verification that can verify patient billing methods instantly at the time of service.
- Claim adjudication
A payer will sometimes run into issues with patient data while a claim is being processed. It could be that there is some incorrect information on the patient’s initial form which causes a problem while settling the claim. In other situations, the patient responsibility may be different from the estimate. Regardless of the type of claim, it’s important that medical practices provide accurate, verified information to payers.
Solving these and other healthcare revenue cycle pain points
The good news: If your practice is facing these challenges, there are solutions available. With the right medical payments system your practice can collect patient information and billing methods upfront, clarify billing confusion, and ensure that payments are automatically processed – even after the time of service.
For more information about how HealthiPASS helps alleviate some of the biggest challenges in the healthcare revenue cycle, contact us today.
{{cta(’24ec6eef-5b67-456a-aaf7-46be961011ca’)}}