Health iPASS automates health insurance verification with real-time eligibility checks through payers, delivering instant coverage confirmation and accurate cost estimates. Reduce claim denials, eliminate manual verification processes, and provide patients with transparent financial information before appointments.
Eliminate administrative bottlenecks, reduce claim denials, and address challenges with uncertain financial responsibility with automated eligibility checks that connect to payers in real time.
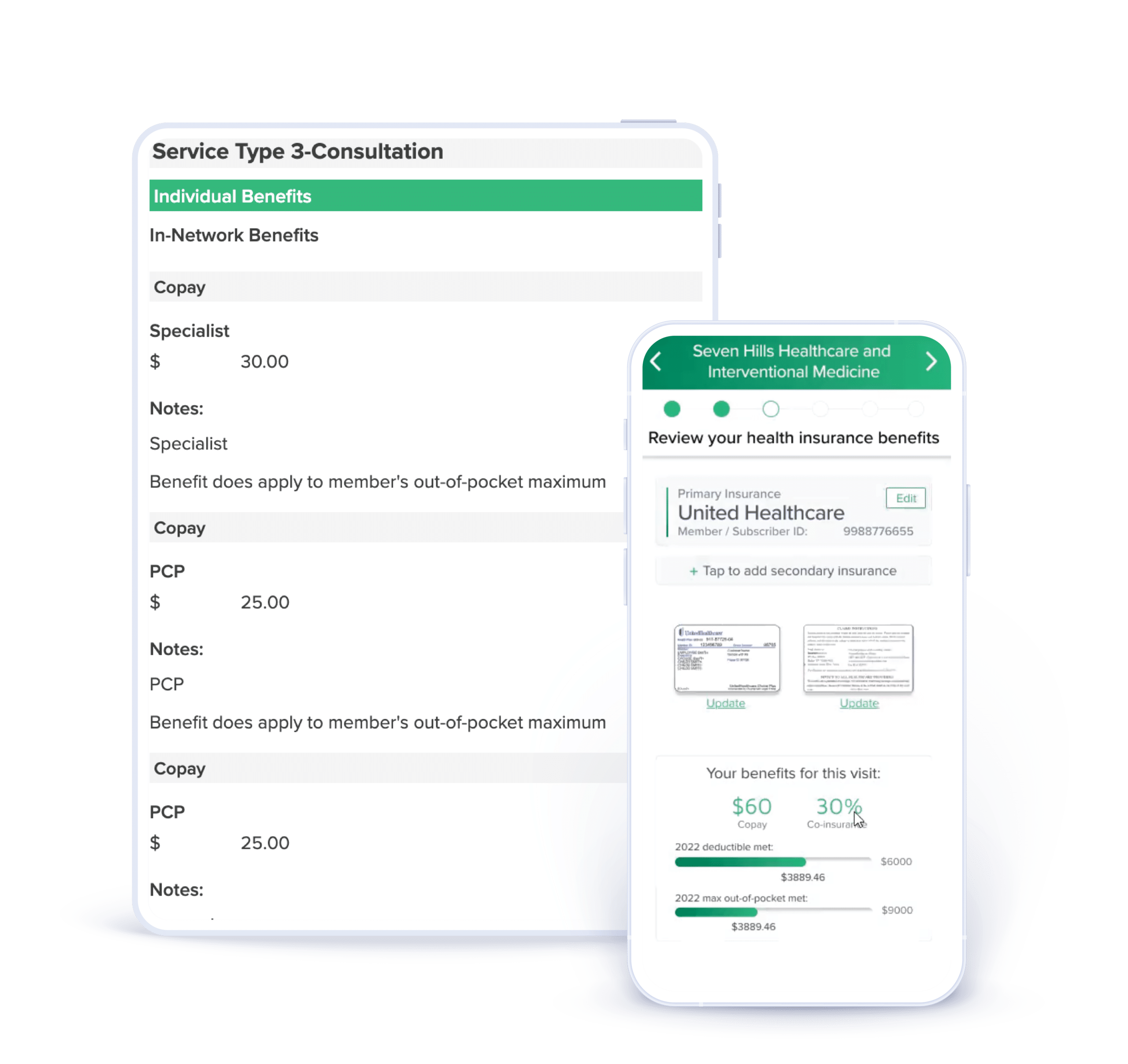
Provide your patients with detailed coverage breakdowns, including copays, deductibles, and out-of-pocket maximums, before appointments, enabling staff to address coverage issues proactively. Bidirectional integration with your PM/EMR system ensures that insurance data flows automatically across all systems, while transparent cost estimates improve patient satisfaction and point-of-service collections.
Patients receive clear benefit explanations and cost transparency during electronic check-in, reducing surprise billing and establishing accurate financial expectations.
Health iPASS eligibility features are available in flexible bundles tailored to your practice’s specific needs and growth stage. Choose from our Connect, Engage, and Accelerate bundles, each offering insurance verification capabilities to streamline revenue cycle management and reduce claim denials.
Explore our key features below.

Automate insurance verification with unlimited real-time eligibility checks across 900+ payers. The rule-based system confirms coverage, copay amounts, deductible status, and authorization requirements before patients arrive, eliminating manual verification delays and reducing claim denials from eligibility issues.
Benefits:

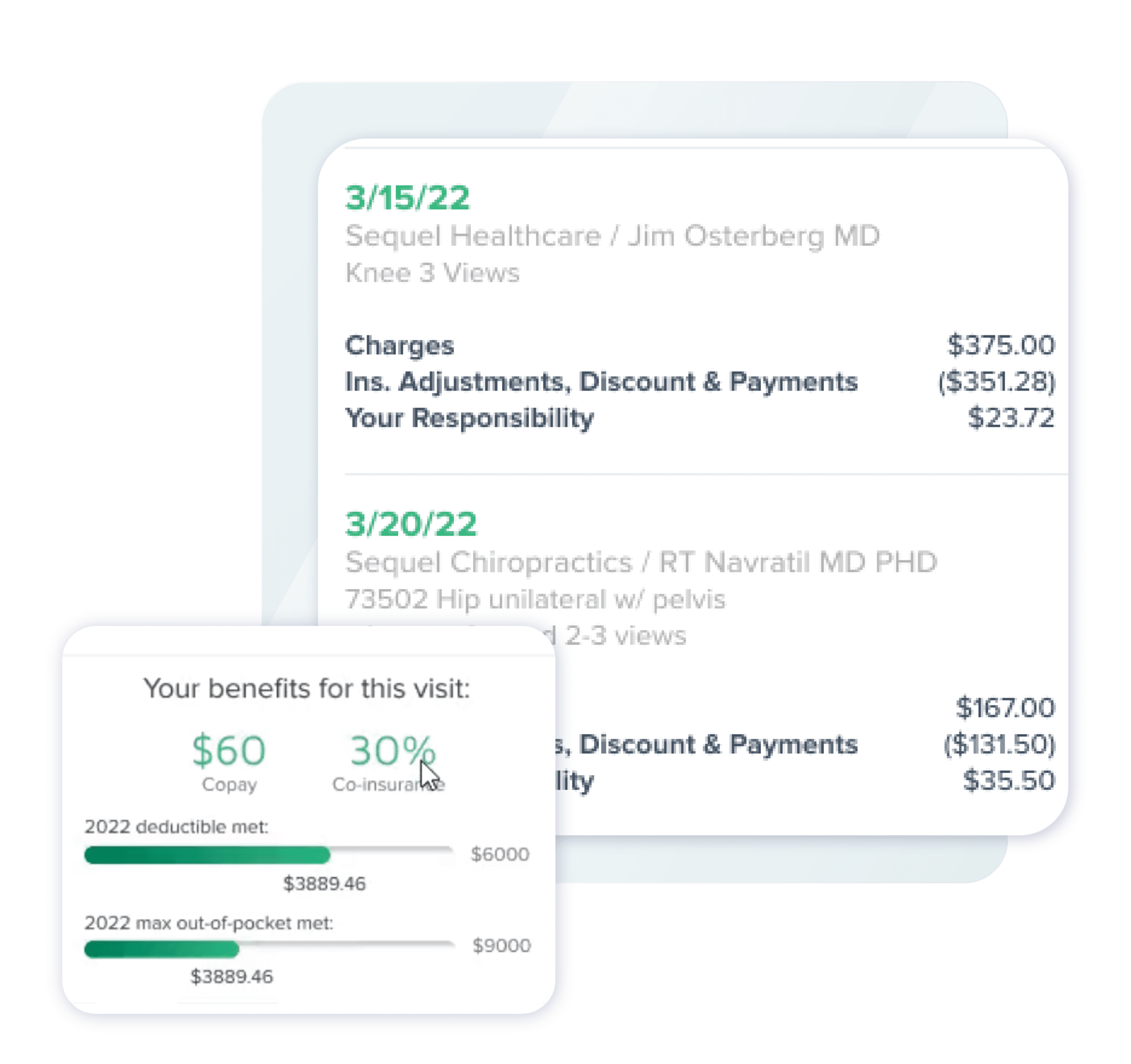
Access comprehensive insurance benefit details, including code-level coverage, copays, deductibles, coinsurance, and out-of-pocket maximums. The platform provides instant visibility into patient financial responsibilities, enabling staff to collect accurate payments at the point of service and proactively address coverage questions.
Benefits:

Deliver transparent out-of-pocket cost estimates during electronic check-in, helping patients understand their financial responsibilities before appointments. The Review of Benefits feature provides simple, clear explanations of insurance coverage tailored to specific appointment types, enabling informed healthcare decisions.
Benefits:

Create customized questionnaires that alert staff to insurance issues, clinical risk factors, or special circumstances during check-in. Pre-screeners can flag conditions such as workers’ compensation claims, insurance verification issues, mental health considerations, or practice-specific clinical protocols.
Benefits:

Insurance verification data flows bidirectionally between Health iPASS and your PM/EMR system, eliminating manual data entry and ensuring consistency across platforms. Verified coverage information, eligibility status, and benefit details automatically sync to your practice management system, while existing patient insurance data pre-populates verification workflows.
Benefits:
Health iPASS links to your PM/EMR and payers via real-time APIs. Insurance data syncs bidirectionally, keeping eligibility, coverage, and benefits updated across platforms. Staff access verification results within existing workflows without switching systems or duplicating data.















Insurance verification integrates seamlessly with Health iPASS payment solutions, creating a continuous revenue cycle workflow. Verified coverage information and accurate cost estimates enable immediate point-of-service payment collection, while transparent benefit explanations improve patient satisfaction and payment compliance.

$200 / provider
Essential eligibility verification for practices establishing automated insurance workflows.
Features Include:
Ideal for: Practices reducing manual verification processes and improving claim accuracy.
$150 / provider
Comprehensive eligibility solution with advanced pre-screening and patient engagement capabilities.
Features Include:
Ideal for: Practices maximizing revenue cycle efficiency with proactive insurance issue identification.
$75/ provider
Financial-focused solution combining eligibility verification with comprehensive payment collection tools.
Features Include:
Ideal for: Practices reducing bad debt and accelerating cash flow through frictionless digital payment workflows.
$100 / provider
Offer your patients a complete pre-arrival solution by combining appointment scheduling and management with any of our other bundle offerings.
Features Include:
Ideal for: Practices optimizing appointment booking and reducing no-shows.
Real-time eligibility verification confirms coverage and benefit details before appointments, reducing denials due to eligibility issues. Automated alerts for out-of-network coverage and expired policies prevent uncompensated care.
Automated insurance verification eliminates phone calls to payers and manual benefit research. Staff access instant eligibility results with detailed coverage breakdowns, reducing administrative time and improving workflow efficiency.
Transparent cost estimates and clear benefit explanations delivered during electronic check-in improve patient understanding of financial responsibilities. Patients arrive informed and prepared, reducing surprise billing and payment disputes.
Accurate cost estimates based on verified coverage enable confident point-of-service payment collection. Detailed visibility into copays, deductibles, and out-of-pocket responsibilities ensures correct payment amounts and reduces billing errors.
Bidirectional PM/EMR integration ensures insurance data remains current and consistent across all systems. Automated eligibility verification reduces coding errors and improves claim submission accuracy, accelerating payment cycles.
Pre-arrival eligibility checks identify coverage issues before appointments, enabling staff to resolve them proactively. Alerts for authorization requirements, referral needs, and payer status changes prevent appointment delays and revenue loss.
See how Health iPASS eligibility verification solutions streamline your revenue cycle, reduce administrative burden, and deliver the transparent cost information patients expect. Our team will help you select the right bundle and features for your practice.